There is a pandemic that is silently spreading across countries and continents. It only indirectly related to the Covid-19 pandemic. The medical journal “The Lancet Respiratory Health” (2024) has an editorial about the inequities of asthma as they develop over the life course. The development of asthma has pre-natal, genetic, environmental, life-style and socio-economic co-determinants. The study of respiratory disease, therefore, is a multi-factorial issue, which needs to disentangle the specific influences. Smoking as well as obesity have an impact on asthma, instantaneously or with delayed time effects of sometimes many years. Hence, it is important to take the whole life course into account, if we want to address the rising disease burden of asthma. Air pollution and heating-up of the planet are important drivers of the silent asthma pandemic across the globe. The social distribution of people working in “asthma- prone” work environments and/or living in highly polluted urban, suburban or rural areas near high frequency traffic is another latent factor causing huge costs to persons and society as a whole. Health inequity is growing over the life course. This is not easy to tackle as policy target as the onset of the disease has no single trigger, but rather a combination of influences that contribute in varying amounts to the evolution of respiratory diseases. (Image air pollution https://aqicn.org/map/germany/de/)

Weight Stigma
The fashion industry has for a long time produced images of mostly women and men that did not correspond to the normal weight distribution of people. Skinny models were present across all media. The so-called social media of today amplify this trend further. The “Barbie hype” has reinforced the idea of low weight as a socially desirable norm. In scientific research the term coined for this phenomenon is “internalized weight stigma” (IWS). A study shows (Highes et al. 2024) it affects more women than men and more people who are described as socioeconomically disadvantaged adults. Pressure to lose weight originates from multiple sources and social media platforms have given rise to bullying. A major outcome of IWS is eating disorders as eating is often wrongly associated to be the only cause of higher weight. It is not. Many other factors contribute to the actual weight of a person. Even the overuse of the body mass index (BMI) as short hand version to define overweight or obesity is misleading for persons with strong muscles. Just fixing on one parameter of body shape or weight tends to reinforce weight stigma. “Keep walking” and a regular healthy diet, this avoids to internalize a weight stigma. Exercise is fun, the more you do it in a group, the easier it is to get going regularly. We ought to keep trying and eventually it will become a routine.

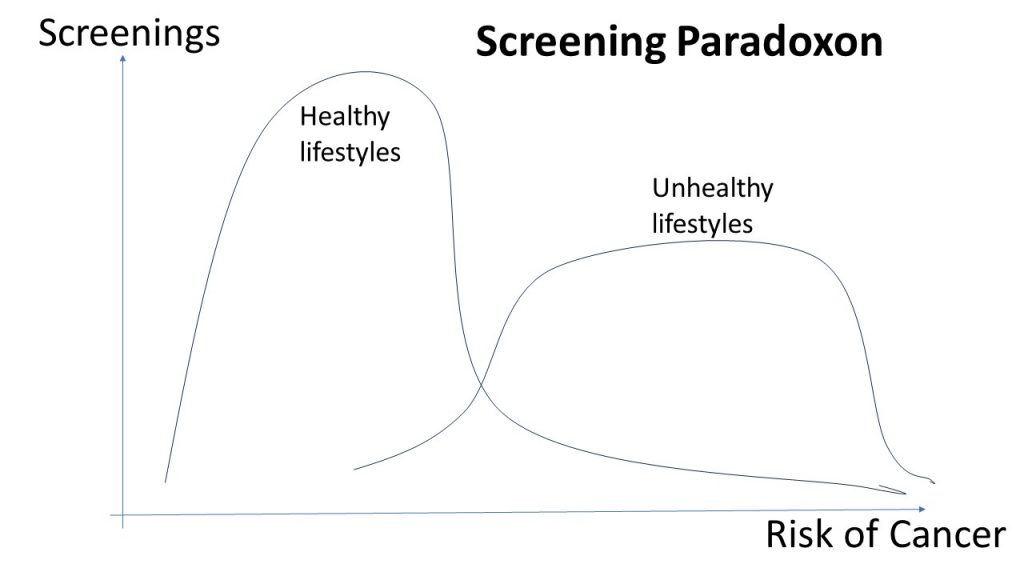
Screening Paradoxon
In the field of public health the screening paradoxon is a well-known feature of large scale programs to check for and contain the large increases in cancer among populations. A recent medical study underscores the necessity to curtail the screening paradox in Europe. The screening paradoxon is defined as “the underuse of screening by those with unhealthy lifestyles and high risks”. The opposite cases, “the overuse of screening by those with healthy lifestyles and low risks” only cause a problem for the costs of the health system as those unlikely of attaining a form of cancer make extensive use of screening. In terms of social inequality we have to be concerned about both ends of these distributions. The publicly available screening programs are skewed towards the higher educated with risk awareness as well as healthy life styles. More of them participate in screening. The other distribution of actual risks and detection of cancer is skewed towards the other end of the risk distribution. The 2 probability distributions overlap to an extent that is most likely co-determined by cultural factors like general attitudes towards prevention.
With the increase in cancer rates generally and due to demographic aging of societies, we shall need to target our resources devoted to health more precisely rather than spending too much on screening of people with very low risks. Increasing the duration between screenings might not impede detection rates of those with healthy lifestyles, but could allow to devote more resources to those people who are hard to reach by screening programs so far. Evaluations of such programs are necessary to judge the need for more targeted programs.(Image own representation inspired by Ola et al. 2024)
Hospital Bias
Asking people about differences between private and public hospitals, you are most likely getting answers that the private hospitals deliver superior patient outcomes. Whereas private hospitals seem to have a positive stigma attached to them, public hospitals commonly have a negative stigma. Scientific evaluations are helpful to set the record straight again. The study published in “The Lancet Regional Health” in 2024 shows that in the simple descriptive statistics on several patient outcome indicators, this is what the data showed between 2026 and 2019. However, a more precise statistical analysis reveals that there is also a selective admission to the private and public hospitals in England. Using so-called instrumental variables approaches that account for the selection process between admission to the 2 types of hospitals (private versus public) most of the differences between the hospital types disappear. The underlying mechanism is a sorting of different patients into the private or public hospitals. Put in easy words, for a routine intervention people tend to chose the private hospital, but the more rare and difficult operations were more likely admitted to public hospitals. The number of co-morbidities (heart disease) is also of importance as they might negatively affect patient outcomes. Jumping to conclusions and reinforcing stigma about public or private provision of services hinders progress and an equitable provision of services.
The analysis of a potential selection bias can reveal the “creaming” effect of private provision of (health) services. Just caring for the “easy” or routine cases and avoiding the more difficult and costly cases has economic advantages, but for society as a whole the costs overall remain the same. A good public service in health is a definite asset.
(Image: Exposition Isa Genzken 2023 in Neue Nationalgalerie Berlin)

Causal Benefit Model
In the field of medicine we move more and more towards precision medicine. Previously, the term of personalized medicine was used which suggested to a certain degree that a personalization might be feasible. The budget constraints have forced us to change the term to avoid unrealistic, untenable promises. In the field of cardiology scientific advances advocate to shift from a risk-based model of treatment to a causal benefit model. (Kohli-Lynch et al. 2024 Link). Long-term benefits of a treatment are more promising, if the treatment addresses the causal mechanisms at work. It is wide spread practice to deal with general risk profiles as guidelines as the precision medicine based on a causal benefit model is far more laborious since to search the causal mechanism at work requires additional testing of hypotheses. This becomes immediately clear if genetic causes enter into consideration. Nevertheless, medical research advances more and more in this direction. Genetic testing has been shown to be useful in analyzing and treating issues like sudden cardiac arrest (in survivors). We are somehow aware that genetics may play a role here, but we shall need a lot of additional studies to make the causal benefit model a feasible option for widespread applications. Targeting research in this field will offer new avenues for precision medicine in the 2020s.
Sleeping BPS-SPB
Sleeping is a good example of the co-determination of the biological, psychological and societal spheres of life. The environment with the daily cycles of light and dark as well as the social norms of work and rest determine the circadian cycles of hormones. Shift work or otherwise disrupted sleep patterns depend on social norms like regulation of noise or light in cities. Healthy sleep patterns, therefore, depend to a large amount on regulation and implementation of those social norms. Birthday parties are tolerated, but much less the irregular partying in shared housing with lots of neighbours. Reducing social contacts during Covid-19 led to the changes in sleep patterns as well.
The psychological determinants of sleep go well beyond the world of dreams as theorized by Freud. Nowadays, we investigate all sorts of behavioural patterns that have an impact on sleeping like “bedtime technology use” of smartphones or the ability to switch off thinking of problems. Sleeping is a particular functional state of our mind. A lot of sorting of daily impressions into memory occurs during the different phases while sleeping. Persistent disrupted or impeded sleep is recognized as torture in severe cases. Stress at work or working overtime is also a major cause of sleep disorders.
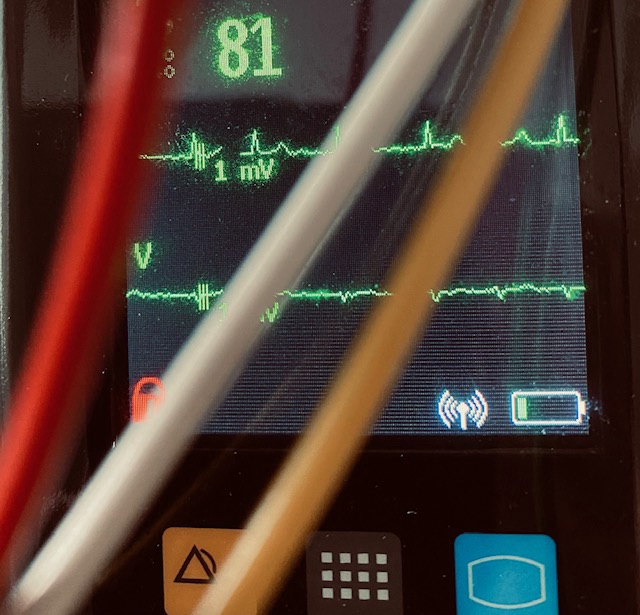
The biological indicators used to investigate sleep have revealed a lot of links of sleep and the hormones of melatonin as well as cortisol. Testing has become more accessible and provides good indicators of how the biological clocks tick within our bodies.
However, we are only at the beginning of the analysis of more complex interactions of the multiple forms of interaction of the bio->psycho->social (BPS) as well as the social->psycho->bio (SPB) co-determination of sleeping. Scientific research is faced with a steep challenge as the direction of causality is not uniform except in very controlled experimental settings. Maybe the arts have coined and popularized a useful term in this respect. “I am in a New York state of mind”.
(Image: extrait of Magritte. La clairvoyance, 1936 and The cultural context of aging, Jay Sokolovsky) 
Sleep biology
Biological processes work hard during our sleep. Our immune system in particular benefits a great deal from undisturbed sleep. This is the simplest summary of the study by Kabrita et al. (2024).
We can study the temporal expression pattern of major histocompatibility complex MHC class I for example in mice. 2 groups of sleep-restricted versus normal mice reveal the biological impact of sleep restriction. In comparison to the control group sleep restriction in mice produced a bimodal pattern of Splenocytes with higher protein levels during the resting period. Such an increased protein expression during resting periods indicates a “preparedness for a potential infection”. Sleep recovery, even if short compared to the longer sleep restriction, allows to return to the baseline of protein levels. The good message is that at least mice seem to recover rather quickly from sleep deprivation with their immune response system.
The biology of repeated phases of longer sleep deprivation could inform us on the implications of sleep deprivation on aging processes. The biological responses in single event sleep deprivation seem to show a fast recovery pattern. Probably it is worth studying the same recovery process of groups of young versus aged mice.
Anecdotal evidence from myself indicates that recovery after sleep deprivation in older humans is no longer as fast as at younger ages. Behavioural responses might be less sleep deprivation (less fun) or longer recovery periods (stay in bed longer). The behavioural response of humans appears to be an obvious one. Instead of either or, we tend to go for both at the same time.
(AI Image: BING +Dall-E. one group of mice is partying in a club at night. Another group of mice is sleeping tight in another room. Cartoon-like images. 2024-3-18) 
Personal Health
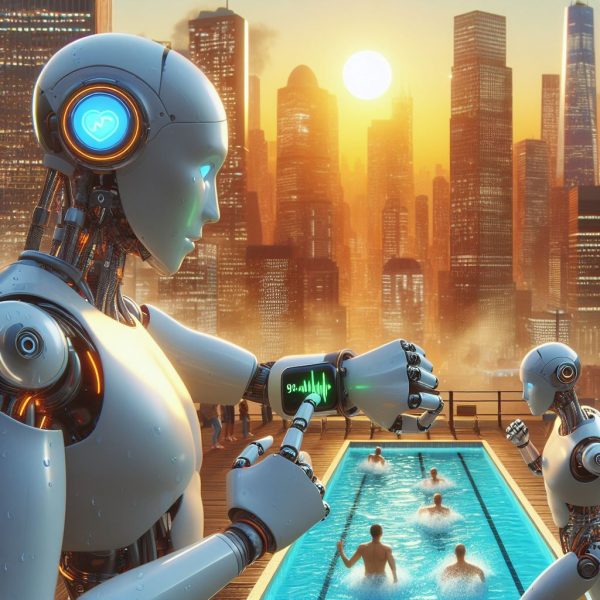
Most people would agree, health is a personal issue. From the onset of life, we have package of genes that predetermine a number of factors of our personal health. Epigenetics has taught us there are many factors to take into account additionally. Environmental factors have huge impacts as well. Improvements in the availability of medical devices in the hands of individuals as well as AI systems on portable devices like smartphones facilitate the monitoring of personal health. Several indicators of early-onset of illness can be retrieved from such devices. Dunn et al. (2024) show that prior to the onset of symptoms of Covid-19 or influenza portable devices can indicate the presence of infections through indicators of resting body temperature, heart rate/min, heart rate variability/millisecond or respiratory rate/min. Combined with the indicators of air quality, indoors as well as outdoors, the presence of allergens a much more personalized data set emerges which can easily be part of an AI-assisted diagnosis. More abundant personal health data and analytical power allows remote and digital health applications to inform patients, medical doctors and the public at large. Digital health technologies are only at the beginning to unfold their potential. Prevention becomes more feasible using such devices, medical professionals should be allowed to focus on interpretation of data and treatment rather than simple data gathering. Thinking about digital health technologies points in the direction of dealing with climate and environmental hazards as sickening causes more forcefully. Personal medicine and personal health are, after all, still heavily dependent on health and safety at work, commuting practices and all sorts of pollution. Personal health, however, is a good starting point to raise awareness of the potentials of digital health technologies to better our lives.
(Image: AI MS-Copilot: 2 robots run in a city. They sweat. The air is full of smog. 2 other robots rest near pool. All look at their wrist watch showing heart beats)